Credits
- Section Writer: [[Dr. Om J Lakhani]]
- Section Editor: [[Dr. Om J Lakhani]]
**Join our WhatsApp channel to get regular updates from “Notes in Endocrinology” and “Endocrinology India”:** [**https://whatsapp.com/channel/0029VaFyQnfHbFUz0LVdBO3****h**](https://whatsapp.com/channel/0029VaFyQnfHbFUz0LVdBO3h)
Support us:
1. [Support you by Becoming a YouTube member (Click here)](https://www.youtube.com/channel/UC6zQSf7dLDqfQOeM4mNUBTQ/join).
- Premium Membership- Download PDF version of Notes, Get ad free video and more
- Consultant Membership- Above plus Download Powerpoint presentation of the notes
2. Support us by purchasing our book - Click here for more details:
- [[Volume 1- THE BEST OF NOTES IN ENDOCRINOLOGY BOOK SERIES]]
- [[Volume 2- THE BEST OF NOTES IN ENDOCRINOLOGY - DIABETES SPECIAL]]
- Video Lecture:
- <iframe width="560" height="315" src="https://www.youtube.com/embed/u3MH1K_Y_zE?si=mGBUKXOllTYgYoSG" title="YouTube video player" frameborder="0" allow="accelerometer; autoplay; clipboard-write; encrypted-media; gyroscope; picture-in-picture; web-share" allowfullscreen></iframe>
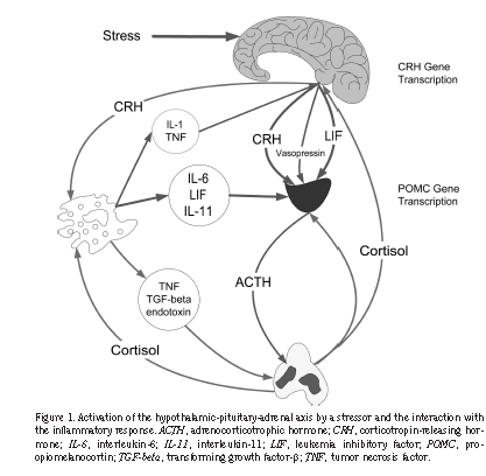
- Q. What are the differences in the HPA axis in Acute vs chronic critically ill patients?
- Acute there is activation of CRH → Increases ACTH→ increases Cortisol
- Chronic → There is suppression of ACTH but cortisol is still high because it is produced by alternate pathways like endotoxins
- Q. What about Aldosterone ?
- Acute illness aldosterone is increased
- Chronic illness→ aldosterone reduced
- **Effects of critical illness on HPA Axis**
- Q. Describe with a diagram, changes in the HPA axis in critically ill patients.
- 
- Q. In terms of absolute values, what are the values of cortisol in normal vs critically ill patients?
- Normal people have cortisol in the range of 5-24 mcg/dl
- In critically ill- they are in the range of 40-50 mcg/dl
- Q. What factors produce an increase in cortisol in critically ill patients?
- Activation of CRH due to stress –main
- Reduction of CBG and albumin increases free cortisol
- Reduced GFR → increase half-life of cortisol
- Inflammatory cytokine → increase peripheral conversion of cortisone to cortisol
- Inflammatory cytokines → increase affinity to glucocorticoid receptors
- Reduced breakdown of cortisol by downregulation of enzymes
- Q. What happens to CBG in sepsis?
- In critically ill patients, CBG reduces
- Hence free cortisol increases
- Half-life of free cortisol is low
- Q. Describe the Negative feedback loop of cortisol in critically ill patients.
- Inflammatory cytokines increase Cortisol → suppress NK-kb transcription → reduce release of inflammatory cytokines
- This is a negative feedback loop
- Q. What are the beneficial effects of glucocorticoids in critically ill patients?
- Increase catecholamine
- Increase blood pressure
- Keep cytokines in check
- Produces insulin resistance both hepatic and peripheral which provides more glucose for another purpose of fighting infection and stress
- **Acute stress **
- Q. Which 2 axes are activated in acute stress?
- HPA axis
- Sympathoadrenal axis
- Q. What is the prevalence of adrenal insufficiency in critically ill patients?
- 10-20% in General
- In septic shock- 60%
- Q. Is there a component of glucocorticoid resistance also?
- Yes
- Some believe that there is a phenomenon called “Systemic inflammation associated Glucocorticoid resistance”
- This is well-known in COPD patients
- In critical illness- ARDS patients tend to have this
- **ASSESSMENT OF ADRENAL RESERVE **
- Q. Is cortisol value associated with mortality in critically ill patients?
- It is controversial and results are mixed
- Both low and high cortisol have been associated with high mortality
- Q. What should be ideally measured in ICU-free cortisol or total cortisol?
- Free cortisol is ideal
- This is because CBG is reduced in critical illness
- However, assays for free cortisol are not reliable and hence free cortisol is not normally tested in ICU
- Q. What is recommended in Williams for assessing adrenal function in critically ill?
- 1. Random Cortisol is done
- a. <15 ug/dl- Insufficient
- b. 15-33 ug/dl- Do SST
- c. If >33 ug/dl- Sufficient
- In SST- Failure of Cortisol to raise by >9 ug/dl- insufficiency present
- These cutoffs are abandoned now, however, they have been used to determine prognosis
- Q. Describe the prognosis based on the results of the ACTH stimulation test.
- Good prognosis
- Baseline cortisol <34
- Rise of cortisol > 9
- 26% mortality at 28 days
- Intermediate prognosis
- Baseline cortisol >34
- Rise of cortisol >9
- Or
- Baseline cortisol <34
- Rise of cortisol <9
- Mortality – 62%
- Poor prognosis
- Baseline cortisol >34 and rise <9
- Mortality – 82%
- Q. Is there any role of low dose ACTH stimulation test?
- Some studies have shown low-dose ACTH stimulation tests to be a better predictor than high-dose
- There are subset of patients with adrenal insufficiency who would be missed by high-dose ACTH stimulation who are diagnosed with low-dose ACTH stimulation
- Q. Does the method of cortisol assay create an issue?
- Yes
- Cortisol measured with LC-MS/MS vs immunoassay has a poor correlation in critically ill patients
- **The Three Situations**
- Q. What are the three different situations that you have to understand while dealing with potential adrenal insufficiency in critically ill patients?
- 1. Patient with underlying Adrenal insufficiency becoming ill - having either adrenergic crisis or increased requirement of glucocorticoids
- 2. Use of Glucocorticoids in refractory septic shock
- 3. CIRCI- "Critical illness-related corticosteroid insufficiency ” (CIRCI)
- 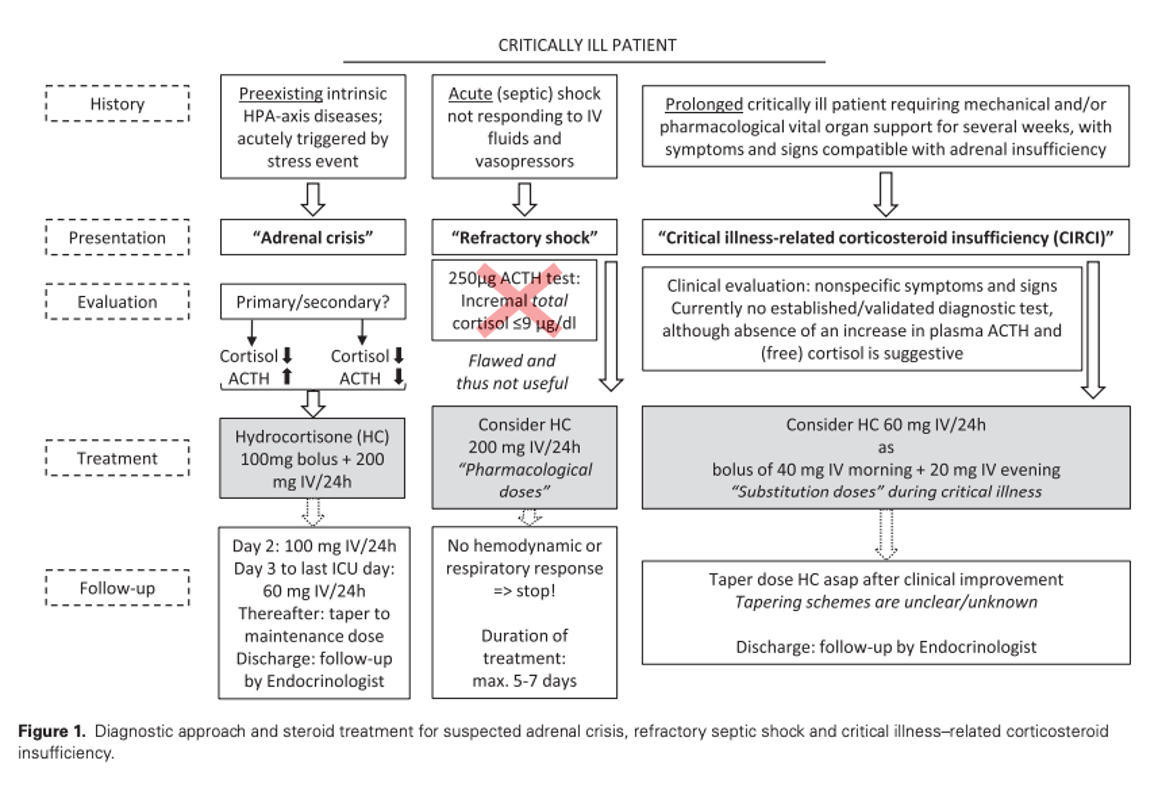
- **Underlying Adrenal insufficiency**
- See notes on [[Diagnosis of Adrenal insufficiency]], [[Treatment of Adrenal insufficiency]]
- Q. What are the causes of adrenal insufficiency in critically ill patients?
- Gram-negative and certain gram-positive infection
- Use of Glucocorticoid use previously and suppression of HPA axis
- Use of certain drugs
- HIV infection
- Adrenal infarct or hemorraghe
- Pituitary apoplexy / Sheehan’s syndrome / other causes of Panhypopituitarism
- Q. Which drugs used in critically ill patients lead to poor cortisol response?
- Etomidate- used for intubation
- Ketoconazole
- Anticonvulsants
- Barbiturates
- Rifampicin
- Q. What is Dr. Om J Lakhani's protocol for diagnosis of Adrenal insufficiency?
- ![[Pasted image 20240210155704.png]]
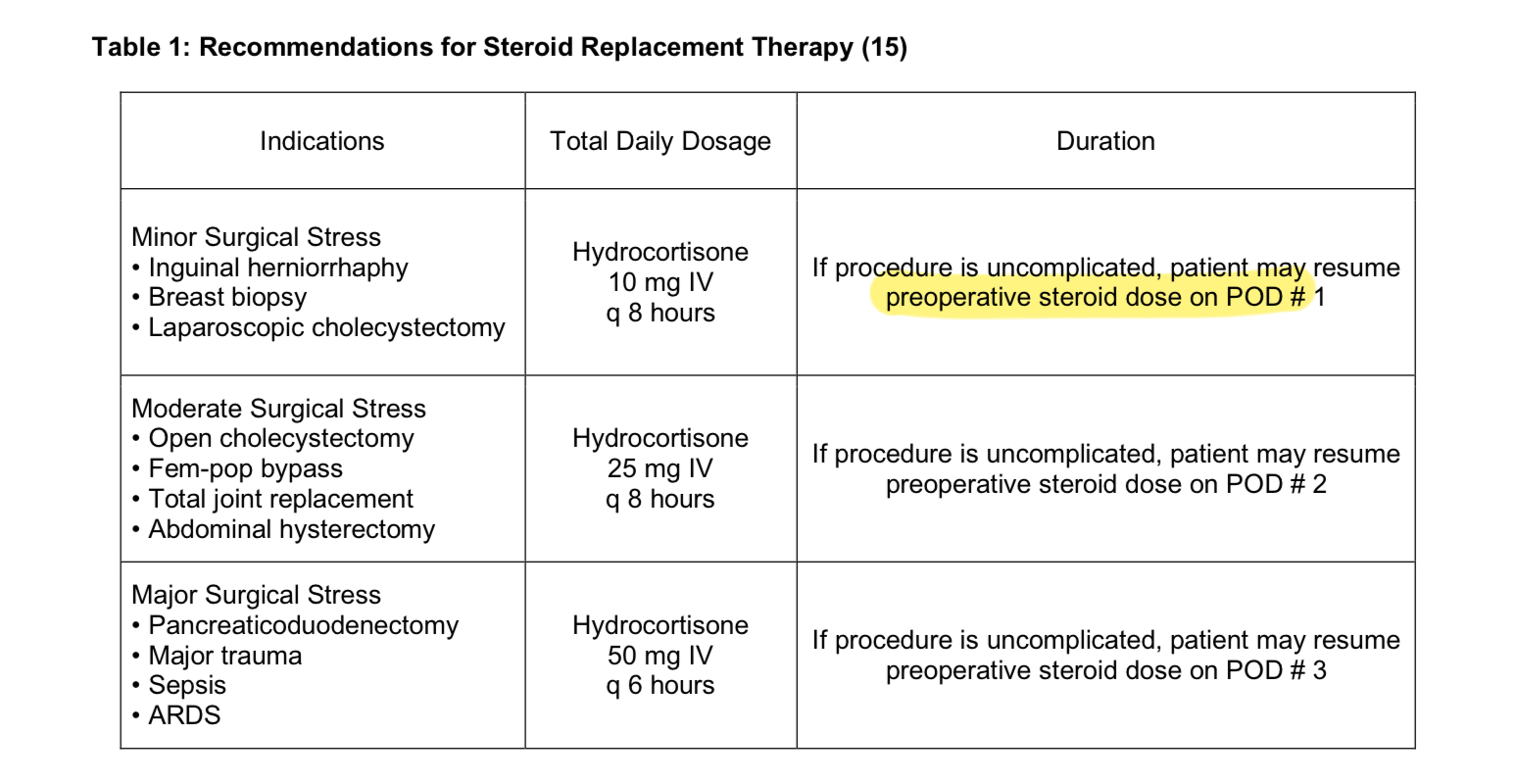
- Q. Recommend preoperative steroid doses in patients with Adrenal insufficiency undergoing surgery?
-
- 
- Q. What is the volume status in primary vs secondary AI?
- Primary AI- volume deficit
- Secondary AI – Normal/ slightly increased volume status
- Hypotension occurs in both cases
- In primary AI it is Mineralocorticoid deficiency leading to volume depletion which is the cause
- In secondary AI → it is lack of pressor effect and lack of Epinephrine which is the cause
- Q. Which is the preferred glucocorticoid in adrenal crisis?
- Hydrocortisone
- Q. Is mineralocorticoid required during an acute adrenal crisis?
- Generally no
- This is because the sodium-retaining ability of fludrocortisone takes 2-3 days to appear
- Saline infusion solves the same purpose
- Hence Mineralocorticoid is unnecessary in acute adrenal crisis
- Q. Describe the emergent treatment of adrenal crisis.
- 1. Establish intravenous access with a large-gauge needle.
- 2. Draw blood for immediate serum electrolytes and glucose and routine measurement of plasma cortisol and ACTH. Do not wait for lab results.
- 3. Infuse 2 to 3 liters of isotonic saline or 5 percent dextrose in isotonic saline as quickly as possible. Frequent hemodynamic monitoring and measurement of serum electrolytes should be performed to avoid iatrogenic fluid overload.
- 4. Give intravenous hydrocortisone, 100 mg immediately, and every six hours thereafter may be used.
- 5. Use supportive measures as needed.
- Q. What is the subsequent management?
- 1. Continue intravenous isotonic saline at a slower rate for the next 24 to 48 hours.
- 2. Search for and treat possible infectious precipitating causes of the adrenal crisis.
- 3. Perform a short ACTH stimulation test to confirm the diagnosis of adrenal insufficiency, if the patient does not have known adrenal insufficiency.
- 4. Determine the type of adrenal insufficiency and its cause if not already known.
- 5. Taper parenteral glucocorticoid over one to three days, if precipitating or complicating illness permits, to oral glucocorticoid maintenance dose.
- 6. Begin mineralocorticoid replacement with fludrocortisone, 0.1 mg by mouth daily, when saline infusion is stopped. (for Primary adrenal insufficiency)
- Q. What type of fluid should be avoided during initial resuscitation of an acute adrenal crisis?
- Avoid hypotonic fluids as they can worsen the hyponatremia
- **Use of Glucorticoids in Refractory septic shock**
- Q. What is the current definition of Refractory septic shock?
- The current definition of refractory septic shock is characterized by the following key points:
- Persistently Low Mean Arterial Pressure: Despite volume resuscitation and titrated administration of vasopressors and inotropes, mean arterial pressure remains low in the context of a proven or suspected infection coupled with organ dysfunction
- High-Dose Vasopressor Therapy: Defined as an inadequate response to high-dose vasopressor therapy, which typically means more than 0.5 mcg/kg/min of norepinephrine or its equivalent
- Association with High Mortality Rate: Refractory septic shock carries a significantly high mortality rate, emphasizing the critical nature of this condition and the challenge it poses in clinical management.
- Q. What was the classical definition used in Clinical trials?
- SBP <90 mm Hg despite 1 hour of adequate fluid and vasopressor administration
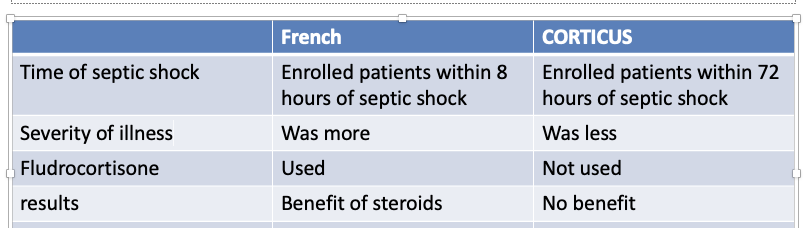
- Q. Describe the FRENCH trial in this area and what were the results.
- The French trial randomly gave critically ill patients a placebo vs Hydrocortisone 50 mg IV /6 hrly + Fludrocortisone 50 mcg
- They enrolled the patient within 8 hours of septic shock
- Before starting they performed 250 mcg ACTH stimulation and defined patients as
- Adequate adrenal reserve- raise of cortisol >9 mcg/dl
- Inadequate adrenal reserve – the rise of cortisol </= 9 mcg/dl
- Results
- Patients in the intervention group had reduced mortality compared to the placebo overall
- Patients having adequate adrenal reserve did not have any difference in mortality compared to placebo
- Patients with inadequate adrenal reserve had more benefits compared to placebo
- Q. What is the CORTICUS trial and what were their results?
- The trial was similar but the results were the opposite
- They used hydrocortisone 50 mg IV /6 hrly with no fludrocortisone for 5 days and then tapered
- They also did the ACTH stimulation and cutoff similar to the French trial
- They found no difference in mortality in the hydrocortisone group
- Q. What was the difference between the French and CORTICUS trials?
- 
- Q. What does meta-analysis show?
- Meta-analysis shows that corticosteroids are more beneficial for patients having severe pressor-dependent septic shock
- Q. What was the APROCCHHS trial?
- In this trial involving patients with septic shock, 90-day all-cause mortality was lower among those who received hydrocortisone plus fludrocortisone than among those who received placebo
- Q. Is corticosteroid beneficial in patients with less severe septic shock?
- No
- Q. How is glucocorticoid administered in eligible patients?
- Hydrocortisone – 50 mg IV /6 hrly (200 mg/day)
An infusion of 10mg/hr can be given, which shows less glucose variability, however, mortality benefits are not known on infusion as most trials done on bolus
- Q. Is fludrocortisone required?
- The COIITSS study found no difference in hydrocortisone alone vs H + fludrocortisone
- Hence fludrocortisone is not recommended
- High dose Hydrocortisone has good mineralocorticoid activity
- Q. How long to give?
- This is not clearly defined
- Generally given for 5-7 days
- not stop abruptly – worsen hemodynamics – taper gradually
- Q. When to taper and when not to taper glucocorticoids for these patients?
- To taper- when steroids used for >7 days → reduced to 50% doses → when hydrocortisone dose is <50 mg/day- can consider adding mineralocorticoid
- When steroid use <7 days- no need to taper
- Q. What is the current consensus about the use of Glucocorticoids in refractory septic shock?
- **Key Points of Consensus**
- **Potential Benefit:** There is evidence suggesting that low-dose, short-course glucocorticoids (specifically hydrocortisone) may offer benefits in refractory septic shock, including:
- Faster resolution of shock
- Reduction in the need for vasopressors
- Potential improvement in survival rates
- **Not a first-line Therapy:** Glucocorticoids are not recommended as a first-line treatment for septic shock. They are primarily used in refractory cases.
- **Dosing and Duration:** Current recommendations favor low-dose hydrocortisone (often 200mg per day) for a short duration (typically up to 7 days).
- **Potential Risks:** Glucocorticoid use comes with potential risks, including:
- Increased risk of infections
- Hyperglycemia (high blood sugar)
- Gastrointestinal bleeding
- **CIRCI**
- Q. Who coined the term CIRCI?
- Marik et al
- Q. Give the concept of absolute vs relative adrenal insufficiency in critically ill patients.
- Absolute adrenal insufficiency – true adrenal insufficiency which is rare and seen in <3%
- Most cases we see in ICU are relative adrenal insufficiency also known as “Critical illness-related corticosteroid insufficiency ” (CIRCI)
- This is the amount of cortisol required considering the critical illness condition is not sufficient
- Q. What is the correct term for relative Adrenal insufficiency in Critically ill patients?
- It should be called “Critical illness-related corticosteroid insufficiency ” (CIRCI)
- Terms absolute and relative adrenal insufficiency are avoided
- Q. What are the diagnostic criteria for CIRCI?
- It is controversial
- However, a consensus guideline by ‘The American college of Critical Care Medicine’ defines it as follows:
- Baseline cortisol <10 mg/dl and/or
- Rise in cortisol </= 9 mcg/dl after high dose ACTH stimulation test
- Q. What values of cortisol rule out Adrenal insufficiency?
- Baseline >34 mcg/dl
- Elevation of cortisol >9 mcg/dl over a baseline value
The above rules out AI in critically ill patients
- Q. What are the conditions in which you should suspect CIRCI?
- Hypotension
- Unresponsiveness to catecholamine infusions
- Ventilator dependence
- Abdominal or flank pain
- High fever with negative cultures and unresponsive to antibiotic therapy
- Unexplained mental changes (i.e., apathy or depression)
- Electrolyte abnormalities (hypoglycemia, hyponatremia, hyperkalemia)
- Neutropenia, eosinophilia
- Nausea, vomiting
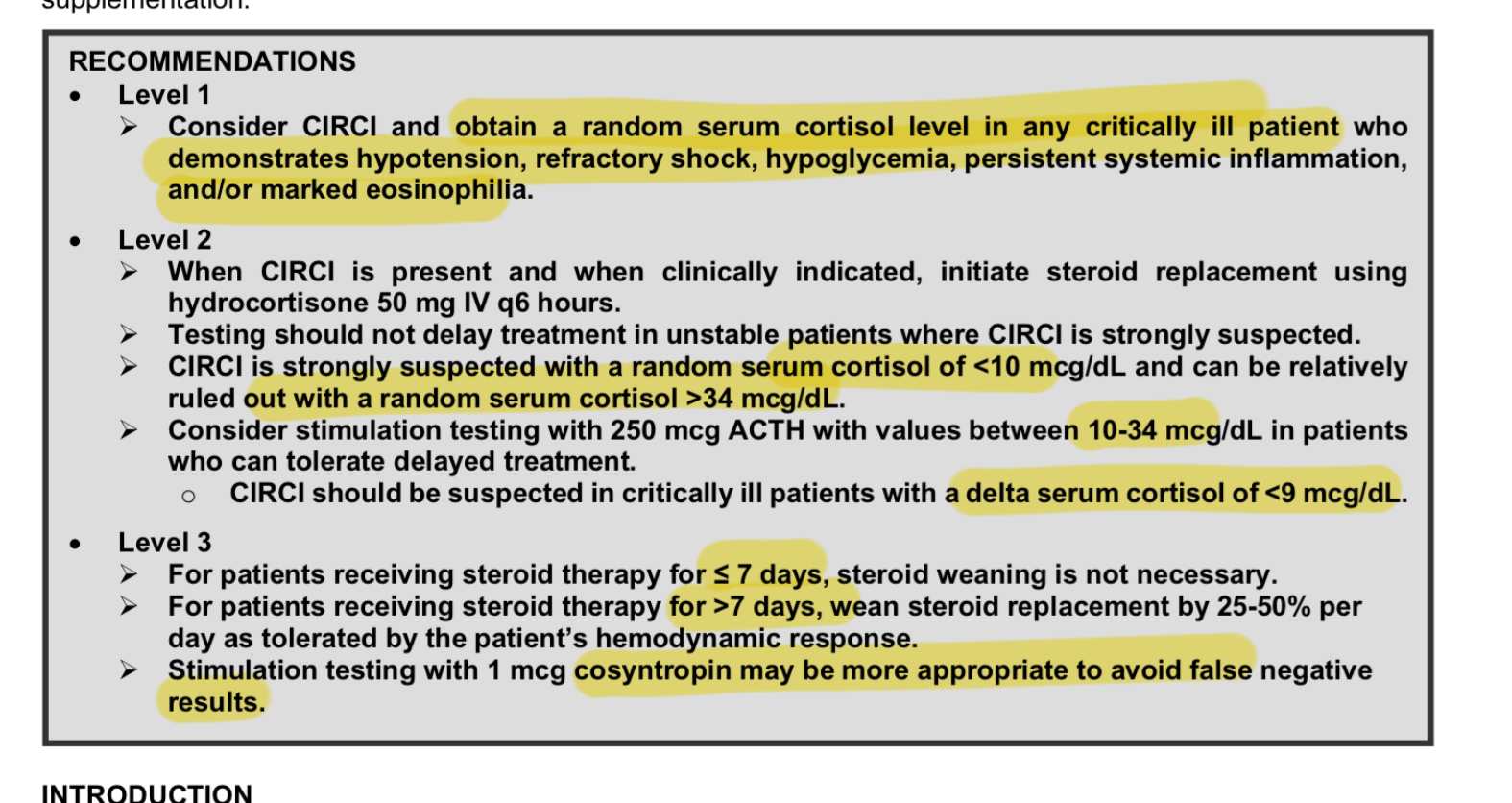
- Q. Give the summary of guidelines from the Surgical Critical Care Net.
- 
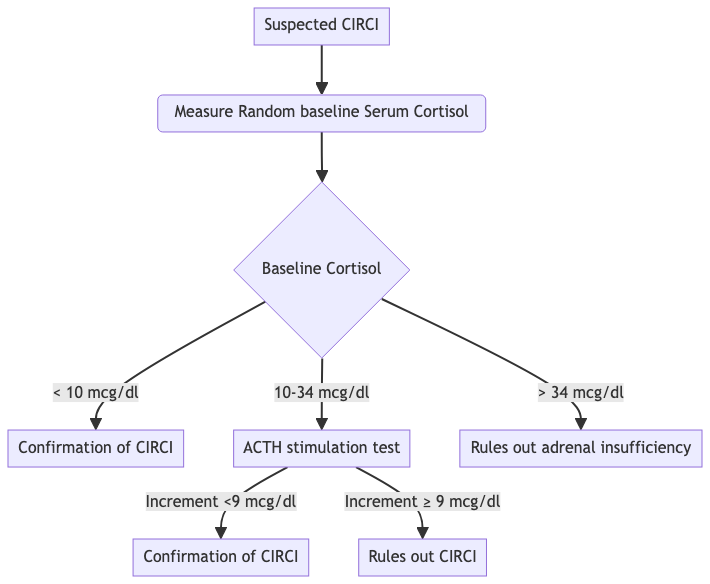
- Q. Summarize the diagnostic criteria for CIRCI with a diagram
- 
- Q. How is ACTH stimulation done in this condition?
- Baseline cortisol
- 250 mcg ACTH is given IM
- after 60 minutes cortisol is repeated
- Q. What is the glucocorticoid dose recommendation for this condition?
- Téblick et al recommend a lower dose in this setting of 60 mg /24 hours
- Q. What is the difference between CIRCI versus other situations in critical illness requiring glucocorticoids?
- According to Téblick, CIRCI is more of a subacute to the chronic situation arising from a longer duration of critical illness
Reference:
1. Téblick A, Gunst J, Van den Berghe G. Critical Illness-induced Corticosteroid Insufficiency: What It Is Not and What It Could Be. J Clin Endocrinol Metab. 2022 Jun 16;107(7):2057-2064. doi: 10.1210/clinem/dgac201. PMID: 35358303; PMCID: PMC9202732.